If you’ve been managing type 2 diabetes for a while, you’ve probably heard the usual advice: check your glucose, watch your diet, get some exercise. But there’s more going on under the surface than just blood sugar numbers.
A new medical review published in Biomedicines (2024) by Dawi and colleagues takes a deep look at what’s really happening inside the body of someone with type 2 diabetes. And it points to something that doesn’t often get talked about: oxidative stress, chronic inflammation, and low levels of a critical antioxidant called glutathione (GSH).
Let’s talk about what that means — in real terms.
What Is Oxidative Stress — and Why Should You Care?
Oxidative stress happens when your body produces more harmful molecules (called ROS, or reactive oxygen species) than it can handle. These molecules damage cells, organs, and tissues over time. For people with diabetes, this damage can pile up — especially in places like:
- The blood vessels (leading to heart disease or stroke)
- The eyes (retinopathy)
- The kidneys (nephropathy)
- The nerves (neuropathy)
In diabetes, high blood sugar fuels this process. The mitochondria — the “batteries” of your cells — get overwhelmed, and that leads to even more ROS being created. Over time, the damage gets harder to reverse.
Where Glutathione Comes In
Glutathione (or GSH) is a powerful antioxidant your body makes to clean up those harmful molecules. Think of it like your body’s built-in cleanup crew. But here’s the catch: people with type 2 diabetes have much lower levels of glutathione, and that puts them at a disadvantage.
According to the review, GSH:
- Helps protect insulin-producing cells in the pancreas
- Supports healthy blood vessels
- Reduces inflammation
- Maintains balance in your cells
But when there isn’t enough GSH — and that’s common in people with T2DM — the body can’t keep up. Oxidative stress builds. Inflammation increases. And diabetes complications become more likely.
Learn more about it here:
👉 Glutathione in Type 2 Diabetes & Microvascular Complications
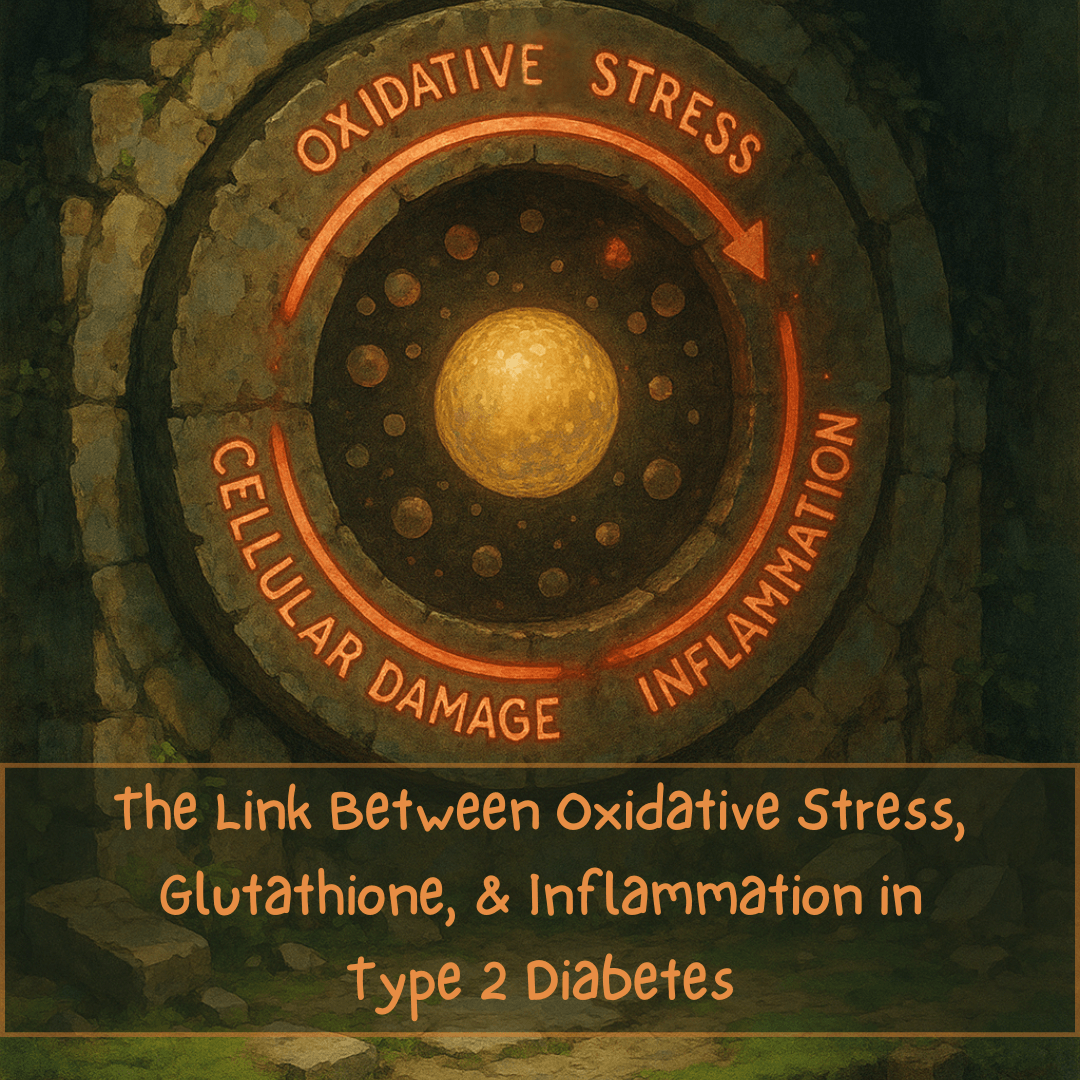
And Then There’s Inflammation
The other big player in this story is inflammation — specifically a molecule called interleukin-6 (IL-6). IL-6 is part of your immune system, but in diabetes, it often gets stuck in “on” mode. It keeps the body in a low-level state of inflammation all the time.
This causes:
- Insulin resistance
- More oxidative stress
- Damage to blood vessels, nerves, and organs
The study found that high IL-6 levels and low glutathione levels tend to go hand in hand — and they make each other worse.
So What Can Help?
Researchers are now looking at two key supplements that may help break this cycle:
1. Glutathione (GSH)
The idea here is simple: if low glutathione makes things worse, restoring it could help. Clinical trials have shown that GSH supplementation can:
- Improve insulin sensitivity
- Reduce HbA1c (a long-term measure of blood sugar)
- Protect pancreatic cells
- Lower markers of oxidative stress
This was especially helpful in older adults with diabetes, who tend to have lower GSH to begin with.
👉 Curious how glutathione helps your heart too?
Read How Glutathione Helps Prevent Cardiovascular Diseases
But there’s a problem: standard glutathione pills often don’t work well. Your stomach breaks them down before they can help.
That’s why liposomal glutathione is gaining traction. It uses a special delivery system that protects the glutathione until your cells can absorb it.
📌 Learn more: Effective Liposomal Glutathione
2. Vitamin D3
Yes, Vitamin D3 — the one you probably associate with bones.
Turns out, it does more than that. The review found that Vitamin D3:
- Reduces IL-6 and other inflammatory markers
- Helps the body make more glutathione
- Improves insulin sensitivity
- May lower fasting blood sugar and HbA1c
And these effects were strongest in people who had low Vitamin D to start with — which includes a lot of people with diabetes.
📌 You can read more or try a trusted source here: Vitamin D3 Supplement
The Bigger Picture
What this study shows — and why it matters — is that treating diabetes isn’t just about glucose. It’s also about protecting your body from damage that builds up silently.
Oxidative stress, low glutathione, and chronic inflammation work together in a harmful cycle. But by supporting your body’s natural defenses — with the right nutrients, lifestyle, and care — that cycle can potentially be slowed or interrupted.
We’re not saying supplements are magic. But if you’ve been dealing with fatigue, nerve pain, slow healing, or other complications, and your labs look okay — this research might explain why you still don’t feel okay.
Final Word
Science is catching up to what many patients already feel: diabetes affects the whole body, not just the pancreas. Understanding how glutathione, inflammation, and Vitamin D3 fit into the picture gives you more tools — and more control — in managing your health.
Talk to your doctor before adding anything new. But if you’re looking for next steps backed by science, this research offers real hope — and practical ways to act on it.
Reference
Dawi J, Misakyan Y, Affa S, Kades S, Narasimhan A, Hajjar F, Besser M, Tumanyan K, Venketaraman V. Oxidative Stress, Glutathione Insufficiency, and Inflammatory Pathways in Type 2 Diabetes Mellitus: Implications for Therapeutic Interventions. Biomedicines. 2024 Dec 26;13(1):18.