BMJ - The Ultimate Tissue Support
BMJ - The Ultimate Tissue Support
$54.95
54.95
BioPro, Inc. and TissueRecovery have closed. What's next?
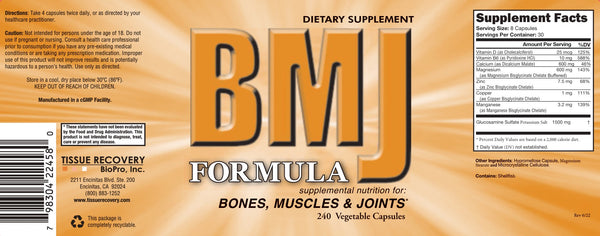
The BMJ Formula
an easy way to effectively support
bone, joints, connective tissue and
neuromuscular function.
This is what Robert S. Hoffman, M.D. says about the BMJ:
I take the BMJ formula myself, and I recommend it to my patients.
The BMJ provides multiple nutrients in a very bioavailable form with benefits documented by research. Bone Included is patented dicalcium malate for improved calcium bioavailability. See the comparison graph. A (Blue-Dicalcium Malate, Red-Calcium Carbonate)
Excerpted and summarized from the full study entitled Comparison of calcium Absorption from various calcium-containing products in Healthy Human Adults: A Bioavailability study. Copyrights, Albion International, Inc. November 2005
Magnesium, copper, zinc, and manganese are included in the BMJ as patented amino acid chelates.
Vitamin D is important for many reasons and it is very common to be deficient or marginally deficient in this vitamin. Vitamin D has been documented to reduce the fracture risk in elderly persons (Bischoff-Ferrari HA, et al. 2009, Bischoff-Ferrari HA, et al. 2005). Vitamin D3 (cholecalciferol) is more efficient in sustaining vitamin D levels. Vitamin D2 potency is less than one-third of vitamin D3 and has a much shorter duration of action compared to vitamin D3 (Armas LA, et al. 2004).
Joints The BMJ contains 1500 mg of glucosamine sulfate in a daily serving which numerous studies have shown to be safe and effective in decreasing osteoarthritis pain (Reginster JY, et al. 2001, Pavelka K, et al. 2002, da Camara CC, et al. 1998, Foster PK, et al. 1995, Pujalte JM, et al. 1980, Drovanti A, et al. 1980, D Ambrosio E, et al. 1981, Lopes VA, et al. 1982.)
The graph below shows research comparing glucosamine sulfate with Ibuprofen for eight weeks (Vaz AL. 1982).
After four weeks the glucosamine sulfate produced more pain relief than the Ibuprofen.
Two studies conducted over three years documented that cartilage degeneration stopped in the treatment group taking glucosamine sulfate while the control group experienced further degeneration (Reginster JY. 2001, Pavelka K, et al. 2002). Research has documented that glucosamine sulfate supplies cartilage with building materials. Glucosamine sulfate caused a significant stimulation of proteoglycan production by chondrocytes (cartilage cells) in samples obtained from human osteoarthritic cartilage (Basleer C, et al, 1998). Another study showed that the treatment of osteoarthritic chondrocytes with glucosamine sulfate resulted in an increased cell-mediated GAG (glycosaminoglycans) content (Dodge GR, Jimenez SA, 2003). GAG is a common building block both for cartilage, ligaments, and tendons. Free radicals are also a factor involved in cartilage degeneration. Patients with osteoarthritis had approximately a four-fold lower level of extracellular SOD, the body owns antioxidant enzymes a constituent of cartilage (Regan E, et al. 2005). Zinc, copper, and manganese are necessary for the formation of SOD. That is one of the reasons these minerals are included in the BMJ. Vitamin D is also important for joints. An increased risk for osteoarthritis of the hip and knee has been documented in people with low-risk levels of vitamin D (Bergink AP, et al. 2009, Lane NE, et al. 1999). Osteoarthritis of the knee and hip progress more rapidly in patients with low vitamin D (McAlindon TE, et al. 1996, Lane NE, et al. 1999). A high percentage of patients with non-traumatic persistent, musculoskeletal pain have been found to be vitamin D deficient (Plotnikoff GA, et al. 2003). Research also shows that support of bone metabolism is important for cartilage integrity. Higher baseline serum osteocalcin, a marker of bone metabolism, has been found to be associated with a decreased rate of cartilage loss (Wang Y, et al. 2005). The BMJ includes important nutrients for both bone and joint metabolism. Vitamin B6 is included in the BMJ because it has shown to help prevent kidney stones when taken with magnesium (Prien E, et al. 1974, Gershoffs, et al. 1967).
The BMJ is now in Vegetable Capsules!
Suggested Use: Take 8 capsules in divided doses daily. ![]()
References: